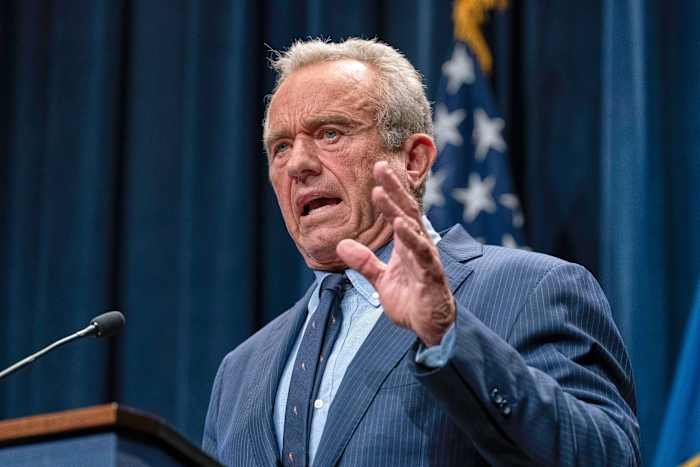
ATLANTA, GA — A federal vaccine advisory committee, known as Kennedy’s vaccine advisory committee, met this week to review and discuss whether newborns across the United States, including right here in Orlando, should continue to receive the hepatitis B vaccine on the very day they’re born. The outcome of this meeting could have significant implications for local hospitals, pediatricians, and families throughout Central Florida.
Background: Why Newborns Receive Hepatitis B Vaccines
Since the early 1990s, the Centers for Disease Control and Prevention (CDC) has recommended that all newborns receive a dose of the hepatitis B vaccine within 24 hours of birth. Hepatitis B is a potentially serious liver infection caused by the hepatitis B virus (HBV). It can be transmitted from mother to child during childbirth, as well as through contact with infected blood or bodily fluids later in life.
The rationale behind early vaccination is to provide immediate protection against infection, particularly for infants whose mothers may not know they are infected. According to the CDC, infants who contract hepatitis B are at a much higher risk of developing chronic infection, which can lead to serious health issues later in life, including liver disease and cancer.
In Orlando, as in the rest of Florida, this recommendation has been widely adopted by hospitals and birthing centers. Newborn hepatitis B vaccination is considered a standard part of infant care, and local medical professionals have followed these guidelines for decades.
The Vaccine Advisory Committee Meeting: What’s on the Table?
This week’s meeting in Atlanta brought together medical experts, public health officials, and community representatives to discuss potential changes to the hepatitis B birth dose policy. The committee is reviewing the latest scientific data on hepatitis B transmission, vaccine safety, and the effectiveness of the current schedule.
Some committee members and public commenters have raised questions about whether a universal birth dose remains necessary in areas with low rates of hepatitis B, or whether targeted vaccination of infants born to mothers who test positive for the virus would be sufficient. Others note that rapid testing during labor is not always feasible, and that the birth dose provides a crucial safety net.
Any changes in these recommendations could impact protocols at Orlando-area hospitals, potentially altering the routine procedures for newborn care at facilities like Orlando Health Winnie Palmer Hospital for Women & Babies and AdventHealth for Women.
Orlando Medical Community Reacts to Possible Changes
Healthcare providers in Orlando are closely monitoring the discussions. Dr. Maria Sanchez, a pediatrician at a leading Orlando clinic, told Daily Orlando News, “The birth dose of the hepatitis B vaccine has been a cornerstone of newborn protection for years. If the guidelines change, we would need to carefully review the new recommendations and ensure parents are well-informed about any updates.”
Local hospitals already follow strict protocols to screen pregnant women for hepatitis B. However, as Dr. Sanchez points out, there are situations where mothers may not receive prenatal care, or test results may be unavailable at the time of delivery. In these cases, the birth dose serves as a vital layer of defense against potential infection.
Some Orlando parents have voiced concerns about vaccines for newborns, citing personal, religious, or philosophical reasons. The advisory committee’s review has reignited discussions among local families about the pros and cons of vaccination at birth.
Potential Impact on Orlando Families and Hospitals
Should the committee recommend changes to the hepatitis B vaccine schedule, Orlando hospitals and clinics would need to update their policies and educate both staff and patients. For families, any new guidance could affect decisions made during those crucial first hours after birth.
Public health officials in Orange County emphasize the importance of maintaining high vaccination coverage to prevent outbreaks. Orlando has a diverse and growing population, including many families who have recently immigrated from regions where hepatitis B is more common. Universal newborn vaccination helps ensure community-wide protection and reduces the risk of transmission.
On the other hand, if the policy shifts to targeted vaccination, local healthcare leaders say it would be vital to strengthen prenatal screening efforts and ensure rapid communication between laboratories, hospitals, and families.
What Comes Next? Timeline for Decisions and Local Input
The vaccine advisory committee is expected to review public comments, scientific studies, and expert testimony before making a formal recommendation to the CDC. Final decisions could come in the next several months, and any changes would likely be rolled out gradually, giving Orlando hospitals time to adapt.
Orlando parents and healthcare professionals can stay informed by following updates from the CDC, the Florida Department of Health, and local medical organizations. Community forums and town hall meetings may also be organized to discuss the implications of any new guidelines.
Conclusion: We Want to Hear from Orlando!
The ongoing review of the hepatitis B vaccine policy for newborns is a reminder of how national health decisions can affect families and providers here in Orlando. Whether you’re a parent, healthcare worker, or community member, your perspective matters. Do you have concerns or questions about the hepatitis B vaccine for newborns? What do you think about potential changes to the guidelines?
Share your thoughts in the comments below and let’s keep the conversation going on this important public health issue in Orlando!